Understand: Chapter 1. PEI: What is it and what’s the issue?
Patients with pancreatic exocrine insufficiency (PEI)
- PEI occurs when the pancreas does not produce enough digestive enzymes1
- Patients with PEI usually present with abdominal pain/discomfort, diarrhoea and unintentional weight loss1
- PEI is a major consequence of numerous other serious conditions (pancreatic and non-pancreatic) including cystic fibrosis, chronic pancreatitis, pancreatic cancer and gastrointestinal surgery. It may also be an important consequence in coeliac disease, irritable bowel syndrome or Crohn’s disease1
- PEI is therefore an extra burden for patients who are already sick
Understand: Chapter 1. PEI: What is it and what’s the issue?
Which patients are at risk of PEI?
PEI may go undetected because the signs and symptoms are similar to those of other gastrointestinal diseases2
PEI frequently accompanies common conditions
Chronic pancreatits3
Pancreatic cancer4
Cystic fibrosis5
Emerging evidence suggests that PEI is also prevalent in:*
Diabetes mellitus Type I6,7**
Diabetes mellitus Type II7,8**
Inflammatory bowel disease10
Coeliac disease11
Diarrhoea predominant IBS12
Crohn’s disease13
*Using faecal elastase screening (discussed further in chapter 2). All studies used cut-off points <200 µg/g FE-1 to indicate potential PEI
**9.2% of diabetes is secondary to pancreatic disease9
Understand: Chapter 1. PEI: What is it and what’s the issue?
Consequences of not identifying patients with PEI
PEI increases the risk of malnutrition, which in turn affects mortality, morbidity and quality of life14
Lack of digestion leads to an inadequate absorption of nutrients1
Left undiagnosed or insufficiently treated PEI can lead to:15
Understand: Chapter 1. PEI: What is it and what’s the issue?
Overview of PEI diagnosis
Professor Domínguez-Muñoz
Director,
Department of Gastroenterology,
University Hospital of
Santiago de Compostela,
Santiago de Compostela, Spain
The views expressed are of the healthcare professional and not the hospital where they work. See Disclaimer for more information.
Understand: Chapter 2. How to address the problem: testing for PEI
Tests are available to diagnose PEI
Patients with abdominal pain/discomfort, diarrhoea and unintentional weight loss should be tested for PEI1
- Several tests are available, which vary in their robustness and cost1
- Although invasive tests are the most sensitive and specific methods to assess pancreatic exocrine function, their cost and invasive nature limit their routine use in clinical practice1
- Non-invasive tests have gained popularity in the clinical setting and will be discussed in further detail
Understand: Chapter 2. How to address the problem: testing for PEI
Tests for PEI
- The British Society of Gastroenterology guidelines on chronic diarrhoea recommend that all clinical centres should have access to at least one non-invasive pancreatic function test, with the faecal elastase being the preferred test18
- Positive screening results for pancreatic disease can be confirmed with various imaging techniques such as endoscopic ultrasound or computed tomography19
Understand: Chapter 2. How to address the problem: testing for PEI
Faecal elastase screening for pancreatic function
Measures the amount of the pancreatic exocrine elastase-1 enzyme in the stool15
Requires a single stool sample and is relatively simple to perform, making this test popular in clinical practice15
Faecal elastase-1 levels are quantified with an ELISA*1
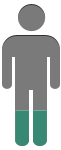
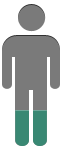
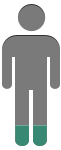
Sensitivity15
| ~100% | in severe pancreatic disease |
| 77-100% | in moderate pancreatic disease |
| 0-63% | in mild pancreatic disease |
Specificity15
| ~93% | (can give false positives in patients with diarrhoea) |
= mild pancreatic disease
= severe pancreatic disease
Understand: Chapter 2. How to address the problem: testing for PEI
Faecal fat test for PEI
Three-day faecal fat test is the gold standard for diagnosing and quantifying steatorrhoea (presence of excess fat in faeces), a key indicator of maldigestion1
The odious nature of this test makes it very unpopular with both patients and laboratory technicians11
Co-efficient of fat absorption is calculated from a 72-hour faecal fat quantification1
Patients keep to a strict diet of 100 g fat/day for 3–5 days Total quantity of faeces excreted during 3–4 days are collected and pooled for analysis
Steatorrhoea is present if the percentage of ingested fat subsequently excreted is:
<7% in patients over 6 months of age
<15%% in patients under 6 months of age
Understand: Chapter 2. How to address the problem: testing for PEI
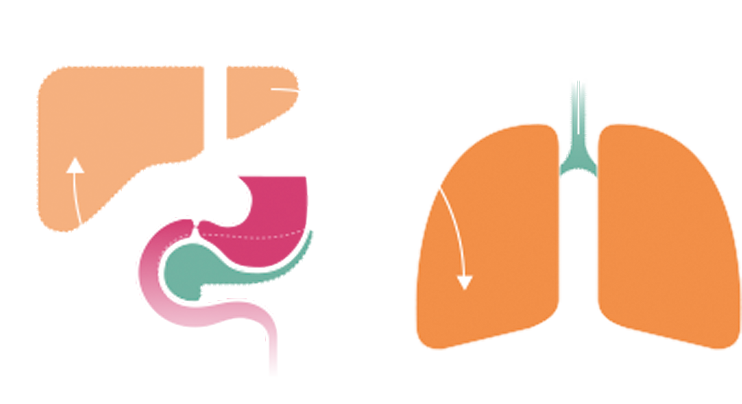
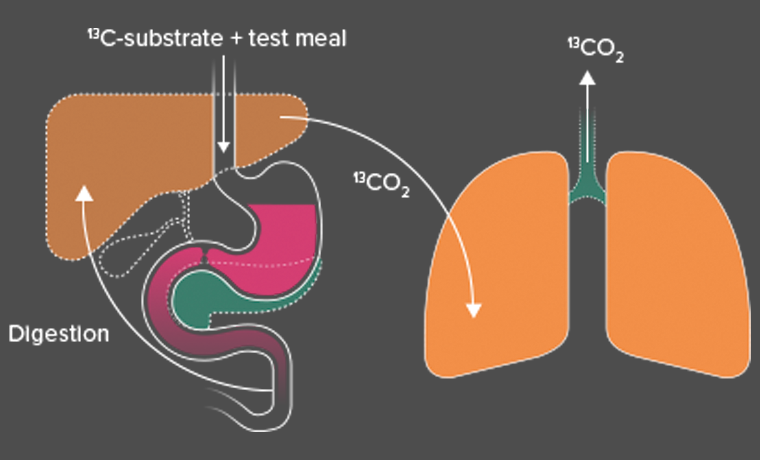
Breath test for PEI
Measures the metabolism of a 13C-substrate by pancreatic enzymes20
This test is easily applicable in clinical practice and is highly robust and reproducible20
A labelled substrate (13C-mixed triglyceride; MTG) is given orally with a test meal20
- A proportion of substrates are metabolised by pancreatic enzymes
- Further metabolism of these products yields 13CO2 which is released with expired air
- The amount of 13CO2 in the expired air can be measured by mass spectrometry or infrared analysis and relates to pancreatic function
Sensitivity for the diagnosis of fat maldigestion is higher than 90%2
How the breath test works
Understand: Chapter 2. How to address the problem: testing for PEI
Overview of PEI testing
Professor Domínguez-Muñoz
Director, Department of Gastroenterology,
University Hospital of Santiago de Compostela, Santiago de Compostela, Spain
Professor David Sanders
Consultant Gastroenterologist, Royal Hallamshire Hospital and University of Sheffield, UK
The views expressed are of the healthcare professional and not the hospital where they work. See Disclaimer for more information.
Understand: Chapter 3. How to address the problem: treating PEI
Pancreatic enzyme replacement therapy (PERT) is the main treatment for PEI1
- Orally administered enzymes facilitate the digestion of fats, proteins and carbohydrates to replace the missing pancreatic digestive enzymes1
- Management of PEI may extend beyond PERT to include the following:21
- Lifestyle modifications (e.g. frequent and low-volume meals, avoiding food that is difficult to digest, limitation of alcohol intake)
- Vitamin supplementation (primarily the fat-soluble vitamins A, D, E, and K)
Understand: Chapter 3. How to address the problem: treating PEI
How does PERT work?22

Understand: Chapter 3. How to address the problem: treating PEI
The correct PERT dose is essential for effective treatment
Dosing varies from individual to individual, depending on the degree of maldigestion and fat content of the meal22
Understand: Chapter 3. How to address the problem: treating PEI
Selecting the correct PERT dose is essential for effective treatment
Dosing varies from individual to individual, depending on the degree of maldigestion and fat content of the meal22
- While different patients may have the same or similar starting doses, the dose should be titrated according to the individual’s response and experience...........

- Abdominal symptoms (those not usually experienced by the patient) or changes in abdominal symptoms should be reviewed to exclude the possibility of colonic damage - especially if the patient is taking in excess of 10,000 units of lipase/kg/day.25,29,30,31
- To help patients understand their dose, they should understand the rationale behind PERT dosing, e.g. the relevance to physiological pancreatic enzyme production24
Understand: Chapter 3. How to address the problem: treating PEI
Overview of PEI testing
Professor Domínguez-Muñoz
Director, Department of
Gastroenterology,
University Hospital of Santiago de Compostela, Santiago de Compostela, Spain
The views expressed are of the healthcare professional and not the hospital where they work. See Disclaimer for more information.
Understand: Optimising management of Pancreatic Exocrine Insufficiency
Now you have completed this section, you should understand:
Which patients are at risk of PEI?
How PEI is diagnosed
How PEI is optimally treated
Early detection and optimum treatment of PEI are essential to relieve symptoms and normalise nutritional status1,26
References
- Toouli J, Biankin AV, Oliver MR, et al. Management of pancreatic exocrine insufficiency: Australasian Pancreatic Club recommendations. Med J Aust. 2010;193:461–7.
- Leeds JS, Oppong K, Sanders DS. The role of fecal elastase-1 in detecting exocrine pancreatic disease. Nat Rev Gastroenterol Hepatol. 2011;8:405–15.
- Dumasy V, Delhaye M, Cotton F, et al. Fat malabsorption screening in chronic pancreatitis. Am J Gastroenterol. 2004;99:1350–4.
- Domínguez-Muñoz JE. Pancreatic enzyme replacement therapy for pancreatic exocrine insufficiency: when is it indicated, what is the goal and how to do it? Adv Med Sci. 2011;56:1–5.
- Walkowiak J, Lisowska A, Przyslawski J, et al. Faecal elastase-1 test is superior to faecal lipase test in the assessment of exocrine pancreatic function in cystic fibrosis. Acta Paediatr. 2004;93:1042–5.
- Icks A, Haastert B, Giani G, et al. Low fecal elastase-1 in type I diabetes mellitus. Z Gastroenterol. 2001;39:823–30.
- Hardt PD, Krauss A, Bretz L, et al. Pancreatic exocrine function in patients with type 1 and type 2 diabetes mellitus. Acta Diabetol. 2000;37:105–10.
- Rathmann W, Haastert B, Icks A, et al. Low faecal elastase 1 concentrations in type 2 diabetes mellitus. Scand J Gastroenterol. 2001;36:1056–61.
- Ewald N, Kaufmann C, Raspe A, et al. Prevalence of diabetes mellitus secondary to pancreatic diseases (type 3c). Diabetes Metab Res Rev. 2012;28:338–42
- Barthet M, Lesavre N, Desplats S, et al. Frequency and characteristics of pancreatitis in patients with inflammatory bowel disease. Pancreatology. 2006;6:464–71.
- Leeds JS, Hopper AD, Hurlstone DP, et al. Is exocrine pancreatic insufficiency in adult coeliac disease a cause of persisting symptoms? Aliment Pharmacol Ther. 2007;25:265–71.
- Leeds JS, Hopper AD, Sidhu R, et al. Some patients with irritable bowel syndrome may have exocrine pancreatic insufficiency. Clin Gastroenterol Hepatol. 2010;8:433–8.
- Maconi G, Dominici R, Molteni M, et al. Prevalence of pancreatic insufficiency in inflammatory bowel diseases. Assessment by fecal elastase-1. Dig Dis Sci. 2008;53:262–70.
- Ockenga J. Importance of nutritional management in diseases with exocrine pancreatic insufficiency. HPB (Oxford). 2009;11(Suppl 3):11–5.
- Sikkens EC, Cahen DL, Kuipers EJ, et al. Pancreatic enzyme replacement therapy in chronic pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24:337–47.
- Vesterhus M, Raeder H, Aurlien H, et al. Neurological features and enzyme therapy in patients with endocrine and exocrine pancreas dysfunction due to CEL mutations. Diabetes Care. 2008;31:1738–40.
- Hardt PD, Ewald N. Exocrine pancreatic insufficiency in diabetes mellitus: a complication of diabetic neuropathy or a different type of diabetes? Exp Diabetes Res. 2011;2011:1–7.
- Thomas PD, Forbes A, Green J, et al. Guidelines for the investigation of chronic diarrhoea, 2nd edition. Gut. 2003;52(Suppl 5):v1–15.
- Choueiri NE, Balci NC, Alkaade S, et al. Advanced imaging of chronic pancreatitis. Curr Gastroenterol Rep. 2010;12:114–20.
- Domínguez-Muñoz JE. Pancreatic exocrine insufficiency: diagnosis and treatment. J Gastroenterol Hepatol. 2011 Mar;26 Suppl 2:12-6.
- Domínguez-Muñoz JE. Pancreatic enzyme therapy for pancreatic exocrine insufficiency. Curr Gastroenterol Rep. 2007;9:116–22.
- Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005 Jul;54(Suppl 6):vi1–28.
- Imrie CW, Connett G, Hall RI, et al. Review article: enzyme supplementation in cystic fibrosis, chronic pancreatitis, pancreatic and periampullary cancer. Aliment Pharmacol Ther. 2010;32(Suppl 1):1–25.
- Domínguez-Muñoz JE. Pancreatic enzyme therapy for pancreatic exocrine insufficiency. Gastroenterol Hepatol (N Y). 2011;7:401–3.
- Creon® 10000 Capsules Summary of Product Characteristics. Available from www.legemiddelverket.no/_layouts/Preparatomtaler/Spc/05-3740.pdf?id=23032015131922.
- Pancreatic exocrine insufficiency. Part 1 of 2: Pathogenic and Diagnostic Considerations. Available from www.gastroendonews.com/download/Pancreatic_CaPart1_WM.pdf. Last accessed 25 June 2013.
- Löhr JM, Oliver MR, Frulloni L. Synopsis of recent guidelines on pancreatic exocrine insufficiency. United European Gastroenterology Journal. 2013;1:79-83
- de-Madaria E, Abad-González A, Aparicio J R, et al. The Spanish Pancreatic Club’s recommendations for the diagnosis and treatment of chronic pancreatitis: Part 2 (treatment). Pancreatology. 2013;13:18-28
- Nutrizym 22 Summary of Product Characteristics. Available from www.medicines.org.uk/emcmobile/medicine/1154/spc Last accessed 2 August June 2013.
- Pancrease HL Capsules Summary of Product Characteristics. Available from. www.medicines.org.uk/emc/medicine/7363/spc Last accessed 2 August June 2013.
- Pancrex V Capsules Summary of Product Characteristics. Available from. www.medicines.org.uk/emc/medicine/1411/SPC Last accessed 2 August June 2013.
- Iglesias-García J, Lariño J, Nieto L, Macías F, Seijo S, Álvarez-Castro A, Villalba C, Domínguez-Muñoz JE. Chronic pancreatitis: A frequent cause of pain-predominant dyspepsia. Pancreatology 2009 (4);9:439.
- Data on file. Abbott Healthcare 2013. RM27509
Disclaimer
Terms of Use
This website is owned by Abbott Healthcare Products Limited (a company with registration number 949253 and its registered address at Abbott House, Vanwall Business Park, Vanwall Road, Maidenhead, Berkshire, SL6 4XE.
Effective Date of these Terms of Use
These Terms of Use and the Privacy and Cookie Policy govern your usage of www.thinkpei.com website controlled by Abbott and its subsidiaries and affiliates (collectively "Abbott").
Scope of Terms of Use.
These Terms of Use only apply to the website located at www.thinkpei.com ("Abbott Website") and do not apply to any other Abbott websites or to third party websites to which the Abbott Website may link. This website is intended for use by healthcare professionals registered within the United Kingdom.
Without prejudice to your rights under applicable law, Abbott reserves the right to amend these Terms of Use (including but not limited to, for the purpose of reflecting technological or functional advancements, legal and regulatory changes or good business practices). If Abbott amends these Terms of Use, we will notify users by posting the amended version with an updated effective date on the Abbott Website. By accessing or using the Abbott Website, you agree to be bound by the then current version of the Terms of Use.
If you disagree with the Terms of Use, your sole and exclusive remedy is to discontinue using the website.
Disclaimer
1. Abbott will take reasonable care to ensure that the information and content on the Abbott Website is accurate, complete, up to date, and always available and does not infringe any third party rights. However, we do not guarantee that this is always the case. The Abbott Website and the content and information on it are provided on an “as is” and “as available” basis, with all faults. To the maximum extent permitted by applicable law, Abbott hereby disclaims all representations and warranties relating to the information and content on the Abbott Website, whether express or implied, created by law, contract or otherwise, including, without limitation, any warranties of merchantability, fitness for a particular purpose, title or non-infringement of third party rights.
2. The information and content on the Abbott Website do not constitute medical advice or guidance in connection with any particular condition. You should consult your healthcare professional, research the subject matter or consult an appropriate expert, before you make any decisions relating to treatment or care of yourself or another person. To the maximum extent permitted by applicable law, Abbott hereby disclaims all liability for any loss or damage which may be suffered by any person, whether suffered directly, indirectly, immediately or consequentially, and whether arising in contract, tort (including negligence) or otherwise which arises out of, or in connection with use of the Abbott Website or any treatment or care decisions which you make, except in the case of death or personal injury resulting from Abbott’s negligence.
3. Abbott is not responsible, and provides no warranty whatsoever, for the accuracy, effectiveness, timeliness and suitability of any information or content obtained from third parties, including any hyperlinks to and from third-party websites.
Your Use
By using the Abbott Website, you agree to the following:
1. Not to disrupt, amend or intercept information posted on the Abbott Website or on any of Abbott’s servers;
2. Not to attempt to circumvent any security features of the Abbott Website; and
3. To abide by all applicable, national and international laws, rules and regulations.
Availability
Abbott will use reasonable efforts to make the Abbott Website available 24 hours a day, 7 days a week. However, we cannot guarantee this and take no responsibility for any loss or damage that occurs due to an interruption of access to the Abbott Website. Abbott may interrupt the Abbott Website for maintenance reasons and will endeavour to provide reasonable notice of any planned events.
Intellectual Property
The information, content and graphics published on the Abbott Website (the "Information") are owned by, or licensed to, Abbott. Permission to use the Information is granted, provided that: (i) the above copyright acknowledgement appears on all copies; (ii) use of the Information is for informational, non-commercial healthcare or personal use only; (ii) the Information is not modified in any way; and (iv) no graphics available from the Abbott Website are used separate from the accompanying text. For all other uses of the Information or any Abbott trademark, trade names or trade dress Abbott’s prior written authorisation is required.
Except as permitted above, no licence or right, express or implied, is granted to any person under any patent, trademark or other proprietary right of Abbott.
Privacy and Security
Abbott is committed to safeguarding your privacy, as set out in the Privacy Policy.
It is your responsibility to ensure that the device used to access the Abbott Website, is adequately secured and protected against malicious software or access by unauthorised persons. To the maximum extent permitted by applicable law, Abbott shall not be liable for any direct, indirect, special, incidental, or consequential damages (including lost profits, whether arising directly or indirectly) suffered by any person as a result of interception or unauthorized access to their personal data, even if Abbott has previously been advised of the possibility of such damages.
Limitation of Liability
Except in the case of death or personal injury caused by their negligence, Abbott, its vendors, their respective directors, employees and agents (hereinafter "Abbott parties") hereby disclaim, to the maximum extent permitted by applicable law, liability for any loss or damage which may be suffered by any person, whether suffered directly, indirectly, immediately or consequentially, and whether arising in contract, tort (including negligence) or otherwise which arises out of, or in connection with: (i) use of, or inability to use, the Abbott Website; (ii) use of information or content on the Abbott Website; (iii) any services provided on or through the Abbott Website; and (iv) interception or unauthorized access to personal information submitted to the Abbott Website, including, without limitation, the following categories of loss or damage, whether or not Abbott has been advised of the possibility of such loss or damage:
(a) loss or corruption of data;
(b) loss of profits;
(b) loss of anticipated savings;
(c) loss of business opportunity;
(d) loss of goodwill;
(e) loss of reputation; and
(f) special damage.
Governing Law
These Terms of Use and the Privacy Policy shall be governed by and construed in accordance with the laws of England and Wales. Any dispute arising under these Terms of Use and/or the Privacy Policy shall be subject to the exclusive jurisdiction of the courts of England.
General
You agree that these Terms of Use, the Privacy Policy and the Cookie Policy describe the entire agreement between us with respect to its subject matter.
Privacy Policy – Effective Date 17th October 2013
This Privacy Policy explains how Abbott Healthcare Products Limited including its subsidiaries and affiliates, (together referred to as "Abbott") handles the personal information that you provide to us on the website www.thinkpei.com ("Abbott Website") controlled by Abbott. Unless otherwise specifically noted, this Privacy Policy does not apply to personal information collected from you offline, to Abbott websites that do not link to this Privacy Policy, to residents of the United States, or to third-party websites to which the Abbott Website may link. Your use of the Abbott Website is subject to this Privacy Policy and the Terms of Use.
Please read this Privacy Policy before using the Abbott Website or submitting personal information to us.
What is "personal information" as used in this Privacy Policy?
"Personal information" means information that identifies you or could be used to identify you and which is submitted to and/or collected by the Abbott Website. Examples of personal information include your name, your postal address, your e-mail address and your telephone number.
How does Abbott collect information online?
Abbott collects information in two ways:
• Personal Information You Submit: Abbott collects personal information that you enter in order to generate an Action Plan. To protect your privacy, you should not provide Abbott with any information that is not specifically requested.
• Cookies: The Abbott Website uses cookies to distinguish you from other users of the Abbott Website. This helps to provide you with a good experience when you browse our website and also allows us to improve our site. For detailed information about the cookies used on this Abbott Website, and the purposes for which we use them, please see the Cookie Policy.
In what circumstances and for what purposes might Abbott collect and use personal information?
Abbott will use the personal information you provide through the Abbott Website to send the Action Plan to you.
Abbott also uses cookies. For detailed information about the cookies used on this Abbott Website, and the purposes for which we use them, please see the Cookie Policy.
Does Abbott consolidate personal information?
Abbott may consolidate the personal information of customers who use Abbott Websites. In addition, we may consolidate information in a non-identifiable form (aggregate/anonymous data) to help us better design Abbott websites, to enhance our research activities, and to facilitate other business functions.
What choices do I have about how Abbott collects and uses personal information about me?
The Action Plan can only be provided to you if you provide us with appropriate personal information.
Abbott Websites that use cookies do not generally provide the ability to opt out of tracking technologies. Some Internet browsers allow you to limit or disable the use of tracking technologies that collect unidentifiable information. However, if you use your browser settings to block all cookies you may not be able to access all or parts of the Abbott Website.
Who will have access to personal information about me?
Personal information can be accessed by a restricted number of Abbott employees, by certain companies with which Abbott may conduct joint programs, and by third parties with whom Abbott contracts to carry out business activities for Abbott.
We train our employees about the importance of privacy and how to handle and manage customer data appropriately and securely. In addition, Abbott’s practice is to require its contractors to keep your personal information confidential and to use your personal information only to perform functions for Abbott.
Does Abbott share personal information with third parties?
Except as otherwise stated in this Section, Abbott will not transfer your personal information to third parties unless you have been provided with an opportunity to opt into this disclosure.
Abbott may disclose your personal information without your opt-in to third party service providers which assist us with our business activities. It is Abbott’s practice to require such third party service providers to keep your personal information confidential and to use your personal information only to perform functions for Abbott and in accordance with Abbott’s instructions.
Abbott further reserves the right to disclose your personal information to respond to authorised information requests from government authorities or when otherwise required by law.
How does Abbott secure personal information?
It is Abbott’s practice to secure the Abbott Website that collects personal information; however, the confidentiality of personal information transmitted over the internet cannot be guaranteed. We urge you to exercise caution when transmitting personal information over the internet. Abbott cannot guarantee that unauthorised third parties will not gain access to your personal information; therefore, when submitting personal information to the Abbott Website, you must weigh both the benefits and the risks. In addition, the Abbott Website will display a warning whenever you link to a website that is not controlled by Abbott; you should check the privacy policies of any third-party website before submitting personal information.
How may I correct personal information or delete it from current customer records?
With your support Abbott will keep personal information accurate and up-to-date. You may request to remove, amend or correct your personal information. Please notify us of your wishes by contacting us in one of the ways specified below.
How long will Abbott store personal information?
In general, Abbott will only store your personal information for as long as it is needed to fulfil the purposes for which it was collected, subject to data retention periods imposed upon Abbott by applicable law.
How can I contact Abbott?
If you have questions about the scope, use, amendment, or deletion of personal information that you have provided to us, or if you would like to opt out of future communications from Abbott please contact by letter at the following address:
Att: Head of Communications
Abbott Healthcare Products Ltd
Abbott House
Vanwall Road
Maidenhead
Berkshire
SL6 4XE
In all communications to Abbott, please include the e-mail address used for registration (if applicable), the Abbott Website address on which you provided any personal information about which you have questions or concerns (e.g. Abbott.com etc.), and a detailed explanation of your request. If you would like to delete, amend or correct your personal information and are contacting us by e-mail, please put "Deletion Request" or "Amendment/Correction Request", as applicable, in the subject line of the e-mail. We will do our best to respond to all reasonable requests in a timely manner.
How will I know whether Abbott has updated this Privacy Policy?
If Abbott changes its privacy practices, an updated version of this Privacy Policy will reflect those changes and we will notify you of such changes by updating the effective date at the top of this Privacy Policy. Without prejudice to your rights under applicable law, Abbott reserves the right to amend this Privacy Policy from time to time to reflect technological advancements, legal and regulatory changes and good business practices.
Cookies
This website uses Google Analytics to help analyse how users use the site. This reporting tool uses Cookies (text files placed on your computer), to collect standard Internet log information and visitor behaviour information in an anonymous form. This cookie information about use of the website is transmitted to Google in USA and stored. We have activated the IP anonymised reporting tool within the website which means that this process will be anonymised (this is known as IP-Masking) and so this information can only be used to evaluate visitors' use of the website on an anonymised basis and to compile statistical reports on website activity. The data will not be mixed with other data. You can deactivate the storage of Cookie Tracking but this website may not work properly. For further information about managing Cookies visit (https://tools.google.com/dlpage/gaoptout) or visit www.allaboutcookies.org.
Video Content
The views expressed in this video are the views of the relevant healthcare professional and do not represent the views of any particular healthcare institution. The views expressed are not the views of Abbott. The information and content of this video does not constitute medical advice and you are strongly advised to consult an appropriate expert, before taking or omitting to take any action relating to your care or the care of another person. To the maximum extent permitted by applicable law, Abbott hereby disclaims all liability for any loss or damage which may be suffered by any person, whether suffered directly, indirectly or consequently and whether arising in contract, tort or otherwise which arises out of or in connection with use of this website or any treatment or care decisions. The information contained in this video is for general information only. Abbott makes no representation, warranty or guarantee whether express or implied that the video content is accurate, complete or up to date.
Action Plan
The content of the Action Plan that will be sent to you is provided for general information only. It is not intended to amount to advice on which you should rely and you are strongly advised to fully investigate the subject matter of the action plan or consult an appropriate expert before taking, or refraining from, any action on the basis of the content of the action plan. Abbott makes no representation, warranty or guarantee whether express or implied that the content of the action plan is accurate, complete or up to date. Except in the case of death or personal injury caused by Abbott’s negligence, Abbott and its respective directors, employees and agents hereby disclaim to the maximum extent permitted by applicable law, liability for any loss or damage which may be suffered by any person, whether suffered directly, indirectly, immediately or consequently and whether arising in tort, contract or otherwise that arises out of or in connection with use of information or content of the action plan.
The development of peripheral neuropathy may be partially explained by mechanisms that are commonly associated with diabetes, although other, non-diabetic mechanisms are also evident16,17
In one study of 54 patients with chronic pancreatitis:15
33% had clinical and laboratory evidence of arterial involvement
15% had electrocardiographic alterations indicating coronary heart disease
22% had peripheral symptoms and signs indicating atherosclerotic disease of the lower extremities
Increased CV risk may result from reduced plasma levels of high-density lipoproteins,
which are protective factors against atherogenesis
Starting doses for infants and children may be calculated based on bodyweight1, 23, 27
< 4 years, 1,000 lipase units/kg bodyweight/meal1
> 4 years, 500 lipase units/kg bodyweight/meal1
Titration may be discussed with the patient when prescribing and at follow up. Extremely high doses of PERT have been reported to be associated with hyperuricosuria and hyperuricaemia25